Background. Allogeneic stem cell transplantation (SCT) with both myeloablative (MAC) and reduced intensity conditioning (RIC) regimens is effective therapyin AML and MDS. However, the relative merits of each may differin different settings and at different time-points after SCT. We have previously reported on the role of dose intensity in a group of 112 patients with AML/MDS given SCT with different regimens between 1999 and 2004 (ASH 2004, Leukemia 2005). At that time we showed that MAC was associated with lower relapse rate, higher non-relapse mortality (NRM) and similar overall survival (OS) as RIC. MAC was associated with survival advantage in patients with active leukemia at SCT. There is paucity of data on the comparison of these 2 approaches very late after SCT (beyond 20 years).
Methods. We have now updated SCT outcomes in the same cohort with a median follow up of 20 years (range, 15-22) in order to better predict long-term outcome and confirm whether late events may have changed the initial conclusions. Updated follow-up is available for all but one patient.
Results. The median age at SCT was50 years (18-70). Eighty-five patients had AML and 17 had MDS (IPSS int2 or high). Fifty-eight hadactive disease at SCT (>10% marrow blasts) and 54 were inremission. The donor was HLA-matched sibling (n=58), 1-Ag mismatchedrelated (n=6) or matched-unrelated (n=48). Twenty-nine patients (26%) had poor risk cytogenetics. Forty-five patients meteligibility criteria for standard MAC and were given intravenous-busulfan (ivBu, 12.8 mg/kg) and cyclophosphamide(BuCy). Sixty-seven patients were considered non-eligible for standardMAC and were given RIC with fludarabineand ivBu (6.4 mg/kg, FB2, n=41) or reduced toxicity conditioning (RTC) with fludarabine and myeloablative dosesof ivBu (12.8 mg/kg, FB4, n=26). The medianage of RIC, RTC and MAC recipients was 57, 51 and 42 years at transplantation, respectively (p=0.001) and a larger proportion of RIC/RTC recipients had unrelateddonors (p=0.01).
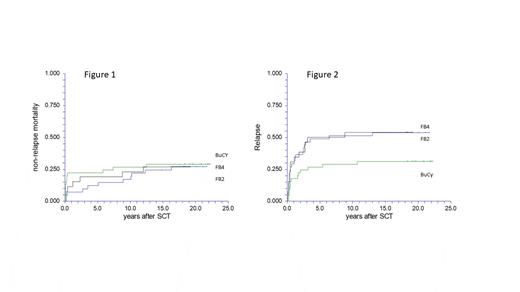
In all, 31 patientsare alive and 81 have died, 50 of relapse and 31 of NRM.The median age at last follow-up was 66 years (35-81). The 20-year OS rate was 29% (20-37). The rate was 40% (26-54), 19% (7-31) and 19% (7-31) after BuCy, FB4 and FB2, respectively (P=0.19). The 20-year NRM was 29% (18-45), 27% (14-51) and 27% (16-45) respectively (Figure 1, P=0.94). The 20-year relapse mortality was 31% (20-48), 54% (38-77) and 54% (40-71), respectively (Figure 2, P=0.12). Five patients with relapse in the first 5 years are very long-term survivors with no recurrent disease following additional treatments.
Forty patients were alive and disease-free 5 years after SCT with a 5-year OS of 42% (33-51). Fourteen patients died beyond 5 years, 3 from late relapse (6.6 -11.8 months after SCT) and 11 due to NRM. The causes of late NRM were second malignancies (n=6), cardiovascular disease (n=3), pulmonary disease (n=1) and liver disease (n=1). The risk of late NRM was 17% (6-47), 25% (7-83) and 44% (24-81) after BuCy, FB4 and FB2, respectively (P=0.29). The risk of late NRM was 14% (4-52) and 35% (21-59) in patients younger and older than 55 years at SCT, respectively (P=0.18). Late relapse mortality was low; 6 (8-37), 13% (2-78) and 7% (1-5), respectively (P=0.81). In all, the subsequent 15-year OS in those who were alive and disease-free 5-years after SCT was 78% (59-97), 63% (29-96) and 49% (22-76), respectively. The small number of events did not allow a meaningful multivariate analysis.
Conclusions. With a long-term follow-up of 20 years, RIC/RTC is an acceptable alternative to MAC in ineligible patients. NRM is lower after RIC in the early post SCT period, but late NRM negates this early advantage and at longer follow-up there is no difference between the regimens. Relapse after RIC is higher at the first 5 years after SCT. However, late relapses beyond 5 years from SCT are rare after all regimens. In all, the very long-term OS is better after MAC. However, older age at SCT for RIC may be a major cause of these observations. Longer follow up of randomized studies is needed for more definite conclusions.
Disclosures
Avigdor:Gilead: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees, Other: Travel/Accommodations/Expenses; Takeda: Membership on an entity's Board of Directors or advisory committees; MSD: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal